By
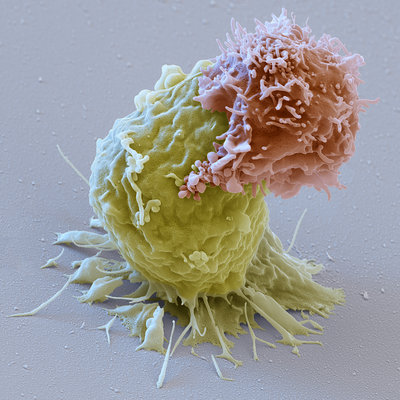
People with high blood pressure can benefit from reducing their blood pressure to levels well below those recommended in current guidelines, according to a new study.
In the study, researchers reviewed information from 42 previous clinical trials and found that treatments that lowered people’s systolic blood pressure to between 120 and 124 mm Hg were linked with the greatest benefits, compared with treatments that didn’t get blood pressure this low. (Systolic blood pressure is the top reading in a blood pressure measurement.)
For example, patients who achieved a blood pressure in the 120-to-124 mm Hg range were 40 percent less likely to die during the study period, compared with those who achieved a blood pressure in the 140- to-144 mm Hg range. Some current guidelines recommend that people ages 60 and older with high blood pressure simply aim to reduce their systolic readings to lower than 150 mm Hg.
The researchers said that their new findings, published today (May 31) in the journal JAMA Cardiology, support the idea of using more aggressive treatment for people with high blood pressure, and they suggest that current guidelines should be revised to recommend lower blood pressure targets.
The study provides “provocative evidence that lower is better,” Dr. Clyde Yancy and Dr. Robert Bonow, of the Feinberg School of Medicine at Northwestern University in Chicago, wrote in an editorial accompanying the study. “The population health benefits of lower blood pressure targets, much lower than we have previously recognized, are real,” they said.
However, other experts say that most doctors will probably wait for new guidelines to come out before changing the way they treat patients.
In addition, it’s important to note that aggressive blood pressure treatments can potentially cause side effects, including electrolyte imbalances and kidney injuries. Thus, doctors should be aware of the risks and monitor patients for side effects, the researchers said. And people who are at a generally lower risk for cardiovascular disease may not require as aggressive of a treatment for high blood pressure as those at higher risk, according to the authors of the editorial, who were not involved in the research.
Lower is better
The new findings touch on a controversial topic — exactly how low patients should aim to go when reducing blood pressure. Guidelines on this issue have been inconsistent. In 2014, guidelines from a government panel of experts, called the Eighth Joint National Committee on Detection, Evaluation, and Treatment of High Blood Pressure raised the recommended blood pressure targets for adult ages 60 and older, from 140 mm Hg to 150 mm Hg. Recent guidelines from the American College of Physicians also recommend the 150 mm Hg target for older adults, but specify a lower target of 140 mm Hg for those with a history of stroke or other risk factors for heart disease, such as diabetes or high cholesterol.
In contrast to these guidelines, recent studies have suggested greater benefits with much lower blood pressure targets. For example, a 2015 study known as the SPRINT trial found that patients who lowered their blood pressure to around 120 mm Hg were 27 percent less likely to die during the study period, compared with those whose treatment target was to lower their blood pressure to less than 140 mm Hg.
But this earlier study involved people who were at particularly high risk of heart problems, for instance, because they already had cardiovascular disease or another chronic condition.
In the new study, researchers at Tulane University wanted to include a larger and more general population of people with high blood pressure. They reviewed information from more than 144,000 people who previously participated in a clinical trial in which they received a high blood pressure treatment or placebo. Participants were followed, on average, for about 4 years.
The average blood pressure that the patients in those studies achieved varied from as low as 114 mm Hg, to as high as 171 mm Hg. In the new study, the researchers compared patients who achieved a blood pressure of 120 to 124 mm Hg to those who achieved a higher blood pressure target, such as 130 to 134 mm Hg, 140 to 144 mm Hg, 150 to 154 mm Hg and 160 mm Hg or higher.
Across the board, those who achieved a blood pressure of 120 to 124 mm Hg had the lowest risk of developing cardiovascular disease, stroke or dying from any cause during the study. For example, even compared with those who achieved a blood pressure in the 130 to 134 mm Hg range, those in the 120 to 124 mm Hg range were 29 percent less likely to develop cardiovascular disease and 27 percent less likely to die during the study period.
Setting a target
In the editorial, Yancy and Bonow recommend that, for people at higher risk of cardiovascular disease, the target should be to get blood pressure down to 130 mm Hg, or lower, if that can be done safely. For those who are at lower risk of developing cardiovascular disease, (particularly those that have difficulty tolerating high blood pressure drugs) the target blood pressure should be 150 mm Hg or lower.
Dr. Arnold Einhorn, a cardiologist and co-director of the Orlando Health Heart Institute who was not involved with the study, said the new findings are strong, and they may prompt doctors to be a little more strict with their patients’ blood pressure numbers. But many doctors will likely wait for new guidelines to come out before they change the way they treat patients, Einhorn said.
One issue with creating new guidelines is that “there are always exception to rules,” and so doctors have to be careful about making recommendations for broad populations, Einhorn said.
The editorial notes that treatments should be a shared decision between a doctor and a patient that takes into account a patients’ particular medical history and health.
The researchers also noted that more studies are needed better determine the outcomes of aggressive blood pressure treatments in patients who have diabetes, and doctors should be particularly vigilant of side effects when treating patients with diabetes or other chronic conditions.
Original article on Live Science.